Welcome to the Blog!
MoM in COVID times
July 3rd, 2020/ Blog post by Mona Mattei, Project Manager
Along with all of you, Mobile Maternity has responded quickly to shift practice in the new virtual world we are operating in for patient care. Yes, MoM has always been a virtual service, but how we can provide tripartite care planning for patients who no longer attend primary care clinics has shifted how we do our care.
Dr Shiraz Moola, Dr. Robin Johnson and their colleagues have added Zoom to their options for patient visits. Zoom Healthcare is not only fully privacy compliant, but it also allows for more than one participant in a patient consult – a primary care physician, or family members who are not nearby – can easily attend with the patient.
Philosophically, MoM holds to the vision of connecting with the regional care provider and collaborative care planning with primary care teams. In our shifting virtual practice, it has been increasingly complex to continue to link with the primary care teams.
Midwifery is particularly suited to the tripartite care planning model as their practice is focused on only maternity care. Interest from the midwifery teams for MoM services has been consistently high throughout the project’s term. With the North welcoming midwives in their area, there is anticipation that they will be connecting with the OBs in Prince George to do MoM type appointments.
With curiosity about what the digital needs are for the maternity provider – provider connections in our province, the MoM team launched a virtual decision support survey for maternity provides in June 2020. Learning about the various needs of the teams across our province in supporting patients and connecting with specialists is critical to next phase planning for MoM and other services.
Please help inform the future of maternity care in B.C. by completing this survey: https://bit.ly/MOMsurvey2020
Check back here for some results as they come in!
MoM North
July 3rd, 2020 / Blog post by Mona Mattei, Project Manager
Spreading the opportunities of Mobile Maternity to our Northern partners, Dr. Raz Moola connected with Dr. Robin Johnson, obstetrician / gynecologist in Prince George to explore options to support rural and remote communities in Northern Interior of BC.
Dr. Johnson has become a champion and lead for the implementation of the Mobile Maternity (MoM) service in the north working with her colleagues Dr. Aaron Kennedy and Dr. Megan Thwaites. In the initial phase, iPads and desktop computers in five communities were set up to be able to connect with the three OBs using a Cisco Jabber meeting room. Family physicians in Burns Lake, Vanderhoof, Fort St. James, MacKenzie and received units and training in June and July 2019.
MoM North holds to the model of tripartite care planning – consults with patients, primary care providers and the specialist. Providing support through the primary care clinics not only enables the physical exams for patients but also ensures that patients had equity of access when they may not have the technology to do virtual visits at home.
Not only do patients have access to obstetrical care for regular consultations, but primary care providers also now have a mechanism to reach out in an emergent situation using the meeting rooms and access through mobile iPads that can be brought into the emergency departments. Primary care providers can connect with the specialist on-call and discuss the case. If needed, escalation to a video is an option for the team.
Next steps for the team are to offer the service to the First Nations community health centers and to grow the referrals from the rural and remote communities that the Prince George team serves.
MoM turns 2!
January 14, 2019 / Blog post by Mona Mattei, Project Manager
Mobile Maternity is celebrating two years of supporting rural moms and families accessing specialist obstetrical care! The next phase of the project will focus on sharing the learnings with other rural communities in the Interior Health Authority and reaching out to Northern Health.
In July 2018, the project team visited 6 MOM communities in the Interior and heard from women and care providers about their experiences. We learnt the value of the ‘safety net’ to specialists access for rural care providers and the convenience expressed by rural woman who benefit a consult with a specialist from their rural location thus eliminating the need for travel. Based on these early indications of success, the MoM project team worked with the Doctors of BC over the fall of 2018 to extend our project timeline and work in new parts of the province using the tripartite care planning model the underpins the MOM framework.
Patients not only save money, valuable time and diminish travel risks but also appreciate the care planning with everyone involved:
“…being pregnant… through winter and driving over that pass in the winter time, I mean I’ve done it a million times but to save that trip… after thinking about it and adding it up it was a couple hundred dollars for sure. Waiting it would’ve been a whole day for me whereas I would’ve had to also take off time, off work, lost wages, all of that”
“..for everything we discussed and questions that came up I want my midwife to be there to hear the answers and hear what we were chatting about and stuff too so having her involved for me was very important. So we’re all on the same wavelength and all talking about the same thing…”
Primary care providers also noted the value of the three-way conversations as key to their engagement in the program:
“We do not have specialists in house to assist with urgent/emergent situations. We also have to appreciate the inability to deliver care during transport, and therefore keep and manage situations that are usually managed by a specialist. With the iPad, we can patch a specialist into the delivery room in real time to assist virtually. Viewing a worrisome strip together is much more effective than trying to fax it piecemeal or describe it over the phone.”
“Absolutely. As a GP surgeon, I find it incredibly helpful to hear how (and which words) Dr Moola obtained surgical consent. I will definitely change my practice by focusing more on this and finding better ways to explain to the patient what we are doing, risks etc.”
Currently, the team is seeking out up to three additional locations interested in spreading the Mobile Maternity model working with their local OB/GYNs. Discussions have taken place with the Central Interior, Thompson regions in the Interior Health Authority and interest has been indicated by the Northern Health Perinatal teams.
Mobile Maternity team is excited to be spreading this great program across our province in 2019!
“Good news, it’s twins,” the doctor said
August 25, 2017 / Blog post by Mona Mattei, Project Manager
On a sunny July day the Mobile Maternity project took its next step in spreading success from the Kootenay Boundary to Vancouver Island.
What began as a random thought by Jude Kornelsen of the Centre for Rural Health Research led the Mobile Maternity team to engage physicians located in Campbell River and the North Island communities of Port Hardy and Port McNeill to explore how the MoM model of care could be used to enhance supports for remote northern Island patients. All agreed the synergies were perfect and the concept for MoM2 was born.
The antinatal period for MoM2 was filled with planning with the Island Health Telehealth team, determining the system – Microsoft Surface tablets for the Island project with Jabber software installed – creating workflows and ensuring ethics were in place for the research project.
In the last week of July, Project Manager Mona Mattei landed with the new tablets to do orientation on the system with the obstetricians and family physicians. There is significant interest in the potential for not only supporting more frequent visits for patients in their perinatal period, but particularly in the opportunity for support in the emergency departments.
-

Port Hardy Physicians and Nurse Practitioner team meet remotely with Dr. Kask in Campbell River
The systems being used for MoM2 are a mix of the Surface tablets and desktop units or existing carts within the facilities. The specialists and one FP – Mat are equipped with the tablets to ensure they can be reached when on-call, where the portability of the units is essential. Port McNeill clinic is equipped with a tablet to enable them to use the units when doing outreach clinics in nearby communities, while Port Hardy is set to use desktop or telehealth rooms.
We are excited to see how the model of care impacts outcomes in a different geographic setting with a varied patient population to support.
-
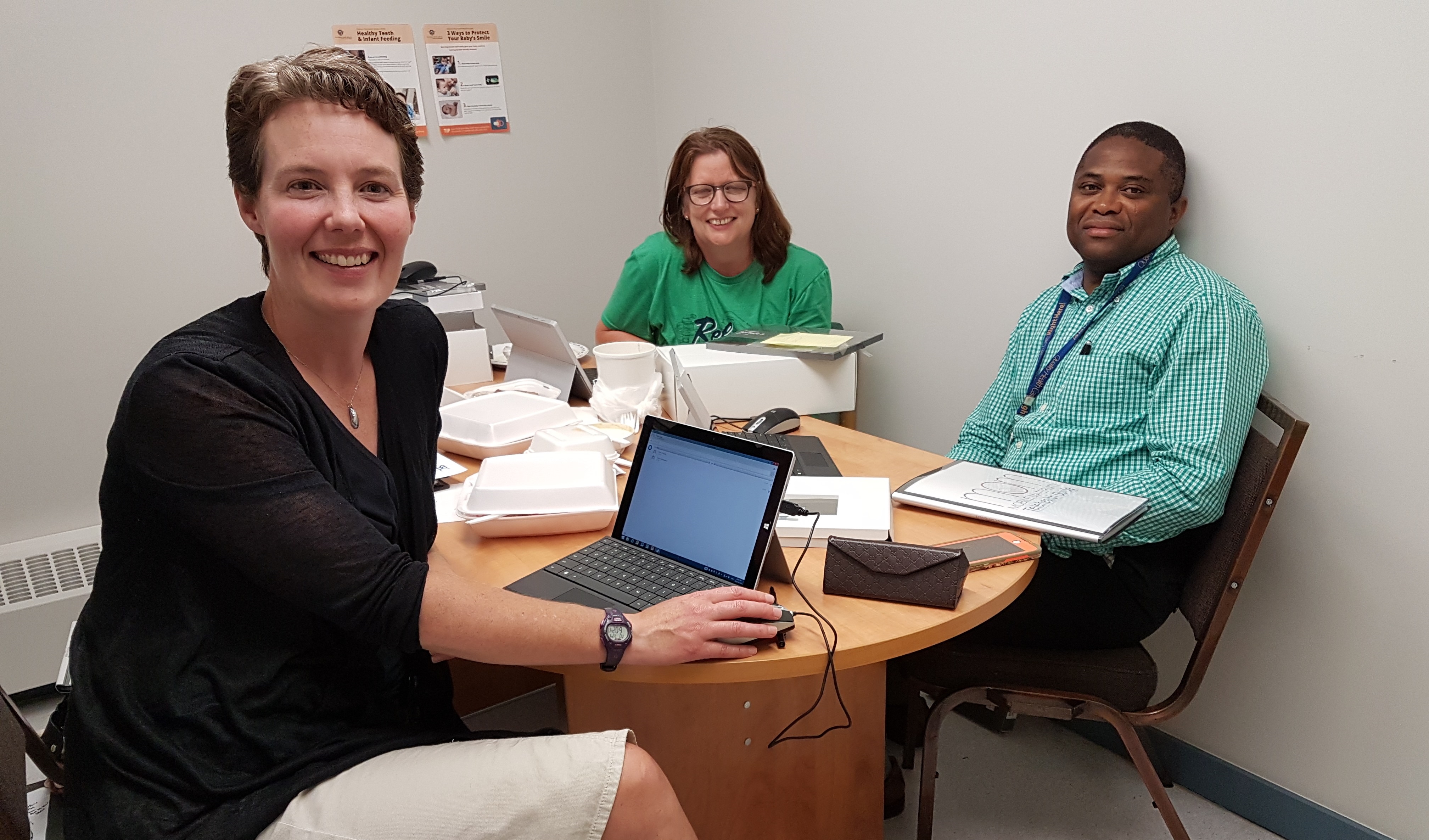
(left to right) Dr. Jennifer Kask, Dr. Kirsten Duckitt and Dr. Remi Adelasoye testing out the new tablets for Mobile Maternity in Campbell River
Welcome to Drs. Adelasoye, Duckitt and Kask in Campbell River who are the receiving specialists and to the family physicians, nurse practitioners and RNs in the North Island communities who have embraced this new service!
The MoM Experience:
This changed my practice…. Interview with Midwife Leah Barlow in Creston
July 1, 2017 / Blog post by Mona Mattei, Project Manager

Leah provides midwifery services in a small town of 5,306 people where the hospital supports C-section deliveries with a family physician group. Midwives deliver in either Creston or Nelson depending on the needs of the clients. Creston is 1.5 hours drive from Nelson with the choice of driving over the highest highway mountain pass in BC or around a lake with ferry services

Dr. Moola began offering the Mobile Maternity (MoM) telehealth service to the area in October 2016. Leah has an iPad that she can take to the patient’s home and connect for a specialist appointment with the client. An important part of the initiative is to include primary care providers in all consults for tripartite care planning.
What my practice was like before MoM:
I work in a rural, remote area so for the women who have any risk factors or need consultation, they would have to leave our community to see a specialist. And for me to find out what the doctor said at the appointment, I’d either get it back in a letter or phone my client. So that puts my clients on the road at all times of the year, through the winter especially.
Sometimes there were delays in receiving information when I needed it. A lot of times I would have to call the specialist when the women were in labour and ask, what about this and this, and try to clear up a question with the consultant. Or else I would call the office to get more clarity on things that I didn’t understand in the letter.
We always seemed to work it out, but things are so much clearer now that the option to connect directly is there.
What my practice looks like now:
Now I offer clients the option to use telehealth to have a consultation with the specialist about a possible risk or complication using the iPad in their home. Occasionally we have done the appointment from the Creston hospital in order to view an ultrasound image or assist in an exam.
When I meet with a client jointly with their obstetrician by telehealth, we can have our plan in place immediately and we all know what to expect or what we can plan around. I feel like it is much clearer for all of us.
I really appreciate being a part of the conversation with the specialist because all of us are on the same page. I know what the doctor said, I know what we need to do next, and what to do for delivery. Because choice of birth site becomes an issue, I don’t know if I need to be in Creston or in Nelson, and we can clarify that at the same time. It really allows for women to have better planning.
Even with technical difficulties at one of the consults, my client said, “It may have taken an hour but if we’d gone to Nelson it would have taken a whole afternoon.” So even with technical difficulties we spent less time than if they had driven. Clients are appreciating that they are not on the road, their partners can be there and he doesn’t have to lose a whole afternoon of work to go with his wife. Partners appreciate that they know what to expect for the birth and can be comfortable with it as well.
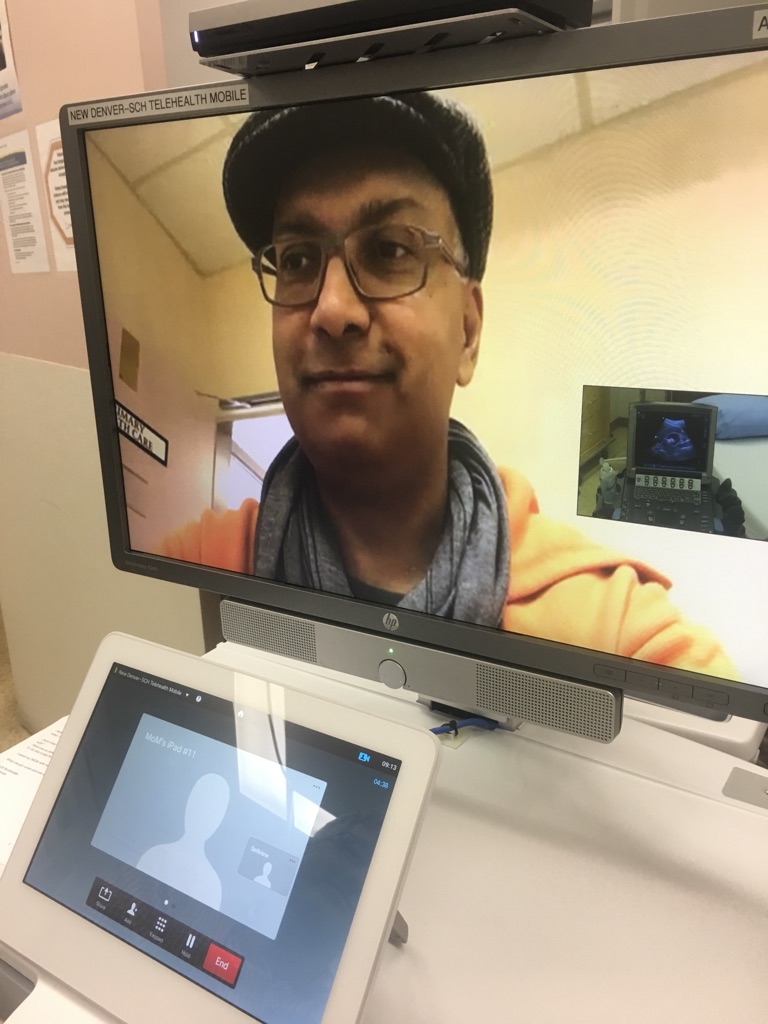
Dr. Moola is able to view Leah’s ultrasound exam and provide feedback in real-time.
The project itself, the quality of the video conferencing is such that you can see and hear well and the clients have all been totally satisfied in feeling that they have had a quality appointment without having to travel. They did not feel that being in front of the specialist in his office would have changed anything at all.
We did an appointment at the hospital and Dr. Moola could watch my exam, see the ultrasound, and was able to confirm the baby was breach. We could make plans without her ever having to travel. I think it has a lot of potential, especially in an acute care setting. Prenatally and in planning for care, it has been incredibly helpful already!
Impact on my practice:
For women, it really improves access to care. I am caring for a woman right now who can’t leave town due to transportation issues, so when I mentioned this she was so excited because financially she couldn’t go, she doesn’t have a car, she’s getting rides just to come to Creston. So, MoM made it possible for her to have a consult. I’ve had difficulties before when women couldn’t leave town and therefore, women didn’t have their consult when they actually needed it. I really love knowing women can get their care no matter what their circumstances!

Leah’s client and her partner use the iPad Pro to meet with Dr. Moola.
From the women, they find that not being on the roads in the winter was, of course safer, but less travel also meant less costs and less problems finding child care. For the women it has many positive effects.
From my side, I love being a part of the team, I like being able to ask the questions even though they seem insignificant and I feel like I walk away feeling that I totally know what to do. I feel it really improves patient care, but also the flow and the continuity of their care. When I can ask questions in the moment of the consult, everything flows smoother for the patient’s care – especially when they need acute care because everybody’s on the same page and has already had that conversation.
I find it really takes the edge off for clients when I talk about a consult now. There’s no hesitation from the client because it’s not going to be a burden on their life.
The ability for women to stay in town to deliver is also very important. When we have a consult conversation through telehealth, women feel like they can stay in their hometown and know that we have support. It is also supportive of our Creston maternity team. We have a great group of doctors who provide C-section coverage – and this project lends support to our services here by helping us keep women in town to deliver if it is possible. It helps us to utilize the strengths of our team here, but to also have backup support if we need it.
The first few weeks….
Nov 16, 2016 / Blog post by Mona Mattei, Project Manager
Once the baby has come it is always a time for adjustments in the family – learning to meet the needs of the new member of the group, how to communicate and testing out new ways of managing life.
Mobile Maternity project manager Mona Mattei, delivered the mobile technology to primary maternity providers in September with orientation on how the new tool can be used. The new member of the family, the iPad, was accepted into the various clinics across the region including: Grand Forks, Creston, New Denver, Kaslo and Nakusp. And the new service was born.
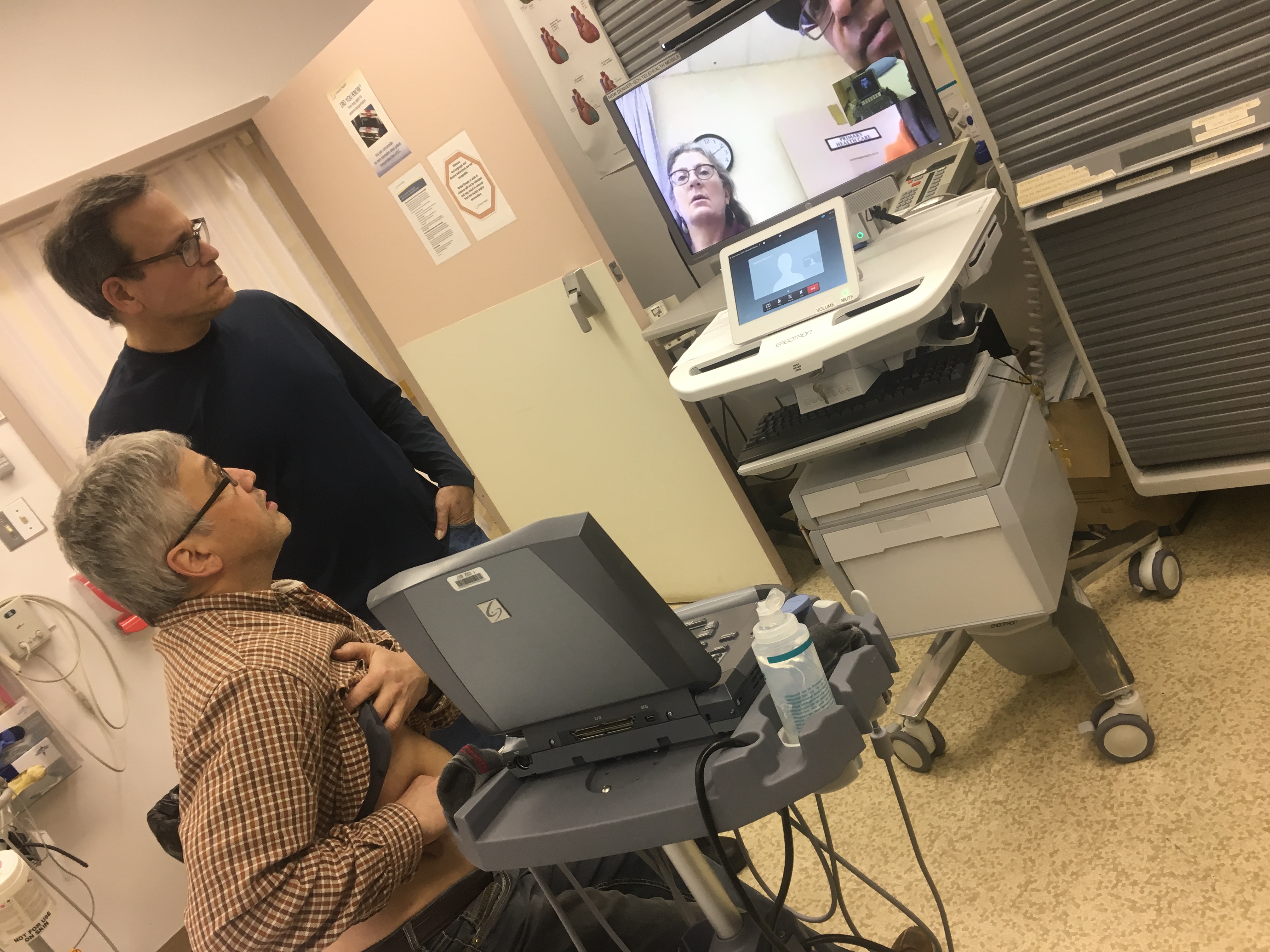
Dr. Shiraz Moola tests out the mobile video conferencing cart in New Denver while Dr. Michael Magier and Dr. Chuck Burkholder demonstrate using the ultrasound equipment. Using an iPad in one location, the system allows physicians to link anywhere within Interior Health including trauma rooms like this one in New Denver.
Dr. Shiraz Moola, obstetrician and project lead, has since seen five patients through his new telehealth service. Each of these patient visits presented a new opportunity to learn. Only one of the five used the mobile technology provided and included a midwife in the visit; it was a scheduled consultation. Three of the next consults were emergent visits where Dr. Moola reached out to the Interior Health Telehealth office to coordinate rooms at different sites for patients to attend and meet with him. These visits have led the team to consider the benefits of coordinating various options for patients to be able to meet with Dr. Moola in different settings.
Curious to hear from the physicians and midwives about their ideas for the new service, Dr. Moola set out on a tour of the region seeking to test out the new communications tool and encourage teams to adopt the new service.
As with most telehealth services, a shift in practice from both the referring practitioner and specialist engaged is critical to the consultation. Remembering to ask for telehealth in referrals, promoting and explaining the service to patients, and taking the time to actually do the visits are all new to providers. Telehealth takes a bit more time for the first while – adjusting schedules, making sure there is extra time in case of technology problems, and extra work on behalf of office assistants.
Yes, learning to incorporate telehealth into practice is a labour of love for doing our work in a different way. It takes champions – specialists, family physicians and midwives to succeed.
Connecting in person was pivotal for Dr. Moola and the providers at the rural sites. Meeting face to face, testing technology and discussing the potential barriers to success were important to building excitement and commitment for this new service.
After 1000 kilometers and nearly 20 hours of travel, Dr. Moola and the team are confident that during the next few months, many patients will be spared the need to do that same amount of travel! Stay tuned to see the baby take its first steps!
First Delivery: Kaslo, Nakusp, and New Denver
Sept 16, 2016 / Blog post by Mona Mattei, Project Manager
With blustery weather of fall upon us, I ventured out into the Kootenay Boundary region feeling a bit like Santa Claus to deliver technology packages for Mobile Maternity. Our first deliveries were to midwives and family physicians north of Nelson in Kaslo, Nakusp and New Denver.
Mobile Maternity, a telehealth research project to enable moms in rural communities to visit with an obstetrician for pre- and post-natal care, officially started on June 1st, 2016. Since inception, it has been the vision of Dr. Shiraz Moola to shift the way that patients access maternity care, by bringing it closer to home. Aiming to ensure that pregnant women are able to see him when they have perinatal risks, and to increase the number of times they are able to visit with him, this project will span over two years tracking the use of the new telehealth service, and how it impacts patients and their babies.
So our first round of deliveries (no not babies… although they feel like newborns) were to the teams around the north Kootenay Lake and Arrow Lake. Small communities between 500 – 1500 people border the lakes and are home to resource workers, tourism staff, and people who like to live a bit off the grid. Many of these women prefer midwifery supports, and there is a group of women in the area who largely refuse medical care, choosing to do unassisted home births instead. Travel to see the OB/GYN can sometimes be a four-hour return trip in challenging weather.
Apple iPad Pros were provided to the GPs and midwives around these areas – a total of 5 in the three locations. These iPads are pre-loaded with a video conferencing system called Real Presence, the designated software that Interior Health Authority (IH) uses. iPads are optimized to pick up IH WiFi signals in any of their locations. All iPads have cellular capability (i.e. data) so in areas where the providers are away from their office, they can still use the iPads.
At the meetings, Dr. Moola linked up with the GPs and midwives using Real Presence while I trained them in how to log into the system and to maneuver their way around the iPads. For some providers, it was the first time seeing Dr. Moola face to face (at least virtually!)
So these iPads are set and ready for patient consults – and potentially emergent care! Next up…. Creston and the surrounding valley, and the Boundary area!
