RSON Background
 The closure of rural surgical and maternity programs in the past 25 years has increased the disparity in access to care between urban and rural residents. Rural Surgical and Obstetrical Networks (RSON) is a way to support safe and appropriate surgery, operative delivery, and maternity care closer to home for rural communities. BC’s Joint Standing Committee on Rural Issues has provided funding over five years (2018- 2022) to support RSONs in eight geographic communities in BC. The networks are supported by five inter-related pillars:
The closure of rural surgical and maternity programs in the past 25 years has increased the disparity in access to care between urban and rural residents. Rural Surgical and Obstetrical Networks (RSON) is a way to support safe and appropriate surgery, operative delivery, and maternity care closer to home for rural communities. BC’s Joint Standing Committee on Rural Issues has provided funding over five years (2018- 2022) to support RSONs in eight geographic communities in BC. The networks are supported by five inter-related pillars:
-
- Increased scope and volume
- Clinical coaching for rural generalists by regional specialists
- Remote presence technology
- Continuous quality improvement
- Evaluation
RSON Evaluation
Overview
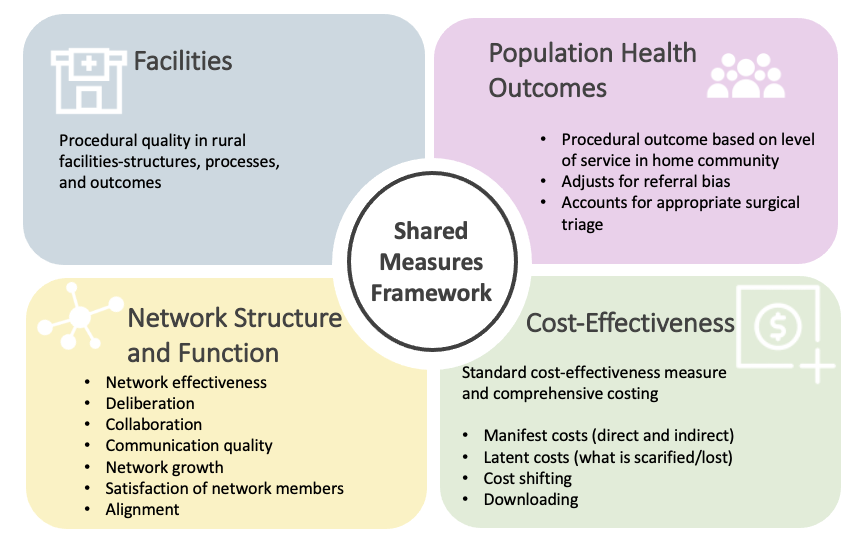
The Centre for Rural Health Research at UBC will design and implement the evaluation of RSON in collaboration with key stakeholders. The evaluation framework includes four streams, all developed using a shared measures framework (Figure 1). This is the first time the RSON model of care is being applied in a Canadian context. For this reason, the evaluation of RSON is critical for iterative network development and improvement. Evaluation findings will also inform other Canadian jurisdictions interested in implementing a similar model of care.
Figure 1. Four evaluation streams developed using a shared measures framework.
Values
 The evaluation is rooted in the following four key values:
The evaluation is rooted in the following four key values:
- Open systems: We respect that networks are dynamic, continuously learning, and self-adjusting.
- Context/difference: We will develop theories using local data that may be transferable to other similar settings. At the same time, we will respect local knowledge in the identification of problems and solutions. Learning will occur across networks and stakeholders.
- Shared measures: We will co-develop indicators with key stakeholders who have expertise in various areas. These stakeholders will also help us develop strategies to address evaluation challenges. Key stakeholders are pentagram partners (Figure 2).
- Pragmatism: We will work with “what is” and not strive for “perfect measures.” We will aim for quality and realistic measures that do not overwhelm health systems.
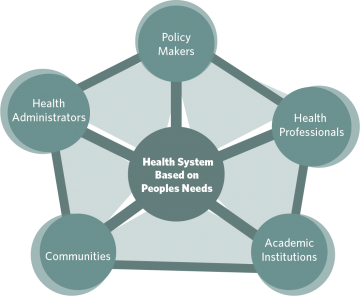
Figure 2. Social Accountability Partnership
Theoretical Approach
The RSON evaluation will be guided by the question, “What works, for whom, in what respects, to what extent, in what contexts/circumstances, why and how?” The program theory and evaluation framework will be modified using emerging evaluation data and feedback from local stakeholders. This will allow for the development of theories that will be specific enough to local networks while also broad enough to be relevant across networks.
RSON Evaluation Midpoint Review
In the past two and a half years, RSON evaluation teams interviewed 21 Administrators, 73 Providers, and 70 Patients.
There are four emerging areas as follows:

Figure 3. Emerging Content Areas
Rural Health Network Profile Tool (RHNPT)
A key component of the evaluation of Rural Surgical and Obstetrical Networks (RSON) is an assessment of network structure and function. This component informs the iterative development of the network and will be useful to other jurisdictions interested in similar network models of care. The network structure and function evaluation stream is comprised of in-depth interviews with central network leaders and an annual survey with the same leaders on organizational aspects of RSON.
Surgical Triage in Rural BC
 Studies show that outcomes are similar for the same procedures performed in small volume surgical programs in rural Canada as large-volume programs. In communities in the Rural Surgical and Obstetrical Network (RSON) project, surgical and obstetrical care is usually delivered by general physicians with enhanced surgical skills (FPESS) and general physician anesthetists (GPAs), with some assistance from regional specialists when needed. In contrast, at larger-volume programs, procedures are typically done by general surgeons. FPESS are required to appropriately triage patients and refer them to regional specialists or local rural care. These referrals occur with discussions between rural service providers and regional specialists, though this process has not been clearly documented. Thus, it is important to document the decision-making behind the triage of patient cases to provide reassurance for the rigour of rural surgical services supported by FPESS. This research aims to highlight and detail the rationale behind surgical triage. Click here to read the summary report.
Studies show that outcomes are similar for the same procedures performed in small volume surgical programs in rural Canada as large-volume programs. In communities in the Rural Surgical and Obstetrical Network (RSON) project, surgical and obstetrical care is usually delivered by general physicians with enhanced surgical skills (FPESS) and general physician anesthetists (GPAs), with some assistance from regional specialists when needed. In contrast, at larger-volume programs, procedures are typically done by general surgeons. FPESS are required to appropriately triage patients and refer them to regional specialists or local rural care. These referrals occur with discussions between rural service providers and regional specialists, though this process has not been clearly documented. Thus, it is important to document the decision-making behind the triage of patient cases to provide reassurance for the rigour of rural surgical services supported by FPESS. This research aims to highlight and detail the rationale behind surgical triage. Click here to read the summary report.
Experiences of Rural Maternity Patients During COVID-19

Few studies have examined the effects of the pandemic on birthing families through a rural lens. Given that the COVID-19 pandemic has in many ways reinforced long-standing disparities between urban and rural communities, it is important that the significance of “place” on the health and wellness of populations is made visible. We set out to understand the maternity experiences of rural families during the early days of the COVID-19 pandemic in order to amplify the voices of those in rural BC communities, and highlight the shared and unique aspects of their experiences. Click here to read the summary report.
Experiences of Rural British Columbians Accessing Surgical and Obstetrical Care
 The attrition of small volume surgical and maternity services in rural Canada over the past three decades has made access to these services especially challenging for rural citizens. While many of these closures have occurred as consequences of regionalization, a strategy to regionally centralize healthcare services, many investigating outcomes of regionalization have focused on cost and medical endpoints rather than the direct experiences of the rural patients affected. In this study, we aimed to understand and document the experiences of rural residence accessing procedural and maternity care both locally and away from home. This study is part of a larger evaluation framework which prioritizes the insight of rural residents regarding healthcare issues. We conducted focus groups and interviews with 54 participants in six communities across British Columbia’s south-eastern and northern regions. Thematic analysis showed that rural residents experienced unique challenges when leaving their communities to access care. This included logistics of travel, poor coordination of care between multiple providers, and financial and psychosocial issues. Despite being mostly content with the medical care received, participants expressed needing more attention to their unique needs and preferences as patients leaving their home communities for care. Understanding these challenges facilitates the planning of healthcare services in a more equitable manner. Our findings suggest that we need increased patient-centered healthcare planning that aims to alleviate the financial and psychosocial strain on rural residents. Click here to read the full report.
The attrition of small volume surgical and maternity services in rural Canada over the past three decades has made access to these services especially challenging for rural citizens. While many of these closures have occurred as consequences of regionalization, a strategy to regionally centralize healthcare services, many investigating outcomes of regionalization have focused on cost and medical endpoints rather than the direct experiences of the rural patients affected. In this study, we aimed to understand and document the experiences of rural residence accessing procedural and maternity care both locally and away from home. This study is part of a larger evaluation framework which prioritizes the insight of rural residents regarding healthcare issues. We conducted focus groups and interviews with 54 participants in six communities across British Columbia’s south-eastern and northern regions. Thematic analysis showed that rural residents experienced unique challenges when leaving their communities to access care. This included logistics of travel, poor coordination of care between multiple providers, and financial and psychosocial issues. Despite being mostly content with the medical care received, participants expressed needing more attention to their unique needs and preferences as patients leaving their home communities for care. Understanding these challenges facilitates the planning of healthcare services in a more equitable manner. Our findings suggest that we need increased patient-centered healthcare planning that aims to alleviate the financial and psychosocial strain on rural residents. Click here to read the full report.
Please email RSON Evaluation Coordinator Shadi Mahmoodi at shadi.mahmoodi@ubc.ca with any questions, comments, or feedback.